
July Tip of the Month - Breaking down Burns
Burns are a frequent presentation in the prehospital environment, ranging from minor surface injuries to life-threatening, multisystem trauma. Accurate identification of the type of burn (thermal, chemical, electrical, or radiation), the depth (superficial, partial-thickness, or full-thickness), and the total body surface area (TBSA) involved is essential for effective triage and timely intervention. Early and accurate assessment guides appropriate fluid resuscitation, pain management, wound care, and transport decisions—including the need for transfer to a burn centre. Prompt recognition and intervention can significantly reduce the risk of complications such as infection, hypovolemia, airway compromise, and long-term disability.
Types of Burns:
• Thermal Burns: Caused by heat sources (flames, scalds, contact)
• Chemical Burns: Exposure to acids, alkalis, or caustic substances
• Electrical Burns: From electric current; may have entry/exit wounds
• Radiation Burns: Sunburn or radiation exposure
• Inhalation Injury: Burn to airways from smoke/toxic fumes
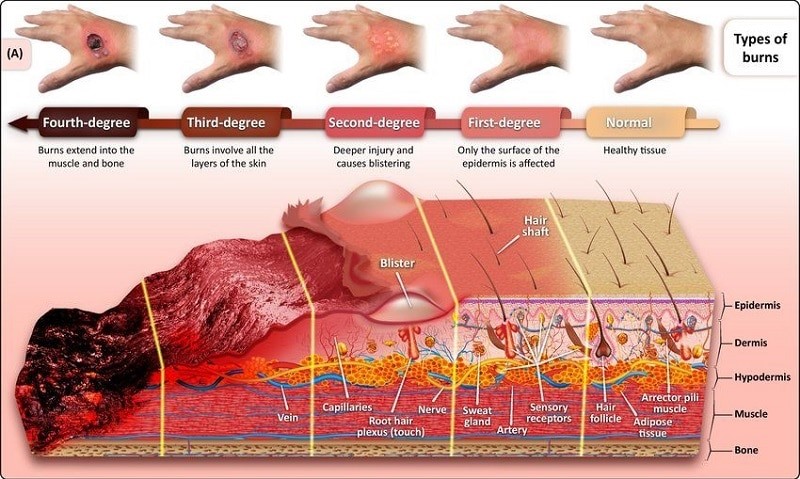
Burn Depth Classification:
• Superficial (1st Degree): Red, painful, no blisters (e.g., sunburn)
• Partial Thickness (2nd Degree): Blisters, moist, painful
• Full Thickness (3rd Degree): Leathery, dry, painless
• Deep Full Thickness (4th Degree): Involves muscle, bone
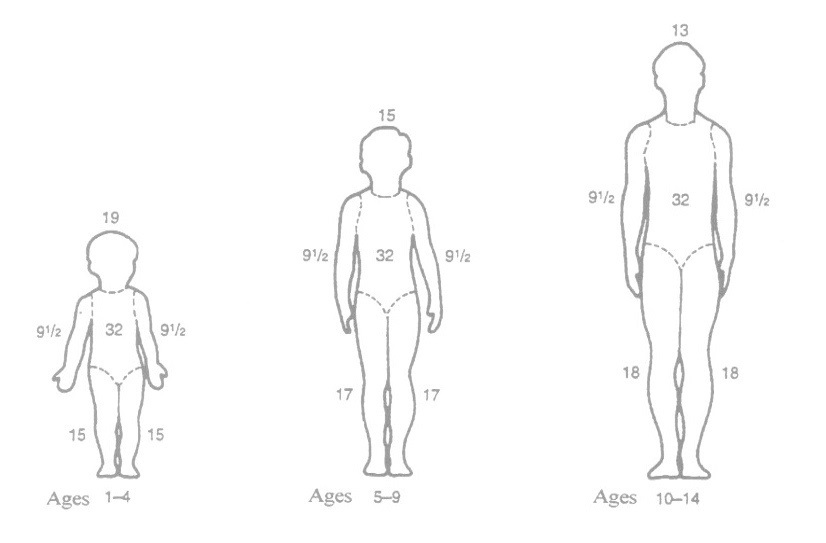
Total Body Surface Area: The Rule of Nines
• Head: 9%
• Each Arm: 9%
• Each Leg: 18%
• Front Torso: 18%
• Back Torso: 18%
• Perineum: 1%
Pediatric Considerations
• Larger head relative to body: Head = 18%, Legs = 14% each
Initial Assessment (ABCs)
• Airway: Look for soot, stridor, hoarseness (early intubation if required and authorized)
• Breathing: High-flow oxygen, monitor SpO2
• Circulation: Check for shock; monitor vital signs
Management
• Attempt to determine the source of burn
• Stop the burning process (cool water, remove clothing)
• Cover with clean dry dressing or sheet
• Pain management (IV analgesia preferred)
• Avoid ice or ointments
• Estimate TBSA
• IV access (preferably in unburned area)
• Transport Early if Indicated
Complications of Burns
Burn injuries are more than just skin-deep. Depending on severity, location, and cause, they can trigger complex systemic responses that lead to life-threatening complications. Timely identification and management in the prehospital phase are critical to improving outcomes. Key complications include:
• Hypovolemic shock
Significant burns disrupt capillary integrity, leading to massive fluid shifts from the intravascular space into burned tissues (third spacing). This results in rapid plasma volume loss, reduced cardiac output, and ultimately hypovolemic shock.
• Infection/sepsis
Burned skin loses its barrier function, making patients highly susceptible to infection. Microbial invasion can progress to sepsis, a systemic inflammatory response with potentially fatal consequences.
• Hypothermia
With skin compromised, burn patients cannot effectively regulate body temperature. Even in warm environments, they rapidly lose heat through evaporation and radiation
• Compartment syndrome
Circumferential full-thickness burns can act like a tourniquet, restricting blood flow and lymphatic return. The resulting increased pressure within a limb or body compartment compromises circulation, leading to ischemia, nerve damage, and tissue necrosis.
• Respiratory distress (especially with inhalation injury)
Burns to the face, neck, or chest—or a history suggesting smoke or chemical inhalation—should raise concern for airway edema, carbon monoxide poisoning, or direct pulmonary injury.
• Renal failure (especially in electrical burns)
High-voltage electrical burns can cause extensive muscle breakdown (rhabdomyolysis), releasing myoglobin into the bloodstream. This pigment is nephrotoxic and can obstruct renal tubules, leading to acute kidney injury (AKI).
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management