
June tip of the month - High-Quality CPR & Defibrillation
Tip of the Month – June
High-Quality CPR & Defibrillation
Paramedics play a vital role in improving survival outcomes for cardiac arrest patients. High-quality CPR and timely defibrillation are cornerstones of effective resuscitation. By maintaining skill proficiency and adhering to resuscitation guidelines, you help optimize perfusion, support neurologic recovery, and reinforce our essential contribution to emergency care.
What Is High-Quality CPR?
According to the Heart and Stroke Foundation, key elements of quality CPR include:
- Chest Compressions: At least 5 cm (2 inches) deep, 100–120 per minute, allowing full chest recoil.
- Minimal Interruptions: Aim for less than 10 seconds off the chest.
- Effective Ventilations: Use a 30:2 ratio with visible chest rise.
- Early Defibrillation: Apply and use the defibrillator as soon as available.
- Compressor Rotation: Switch every 2 minutes to avoid fatigue and maintain compression quality.
Pediatric Considerations
When to Start CPR:
Initiate chest compressions in infants and children if:
- The patient is vital signs absent
- The heart rate is < 60 bpm with signs of poor perfusion, despite adequate oxygenation and ventilation.
This recommendation aligns with the AHA PALS Guidelines (2020 & 2023 updates) and reflects the fact that pediatric cardiac arrest is often secondary to respiratory failure or hypoxia, not primary cardiac causes.
CPR Compression-to-Ventilation Ratios:
- Single rescuer: Use a 30:2 compression-to-ventilation ratio.
- Two rescuers: Use a 15:2 ratio to improve ventilation support.
✅ Remember: Children need more frequent ventilation than adults due to higher oxygen demand and lower functional reserves.
Compression Depth:
- Infants: About 4 cm (1.5 inches) — or one-third the depth of the chest.
- Children: About 5 cm (2 inches) — also one-third the depth of the chest.
Compression Technique:
- Infants: Two fingers (single rescuer) or two-thumb encircling hands (two rescuers).
- Children: One or two hands on the lower half of the sternum, as appropriate for the child’s size.
Defibrillation & Pad Placement
Why Pad Placement Matters:
- Ensures current flows through the heart for optimal shock efficacy.
- Minimizes risk to surrounding tissues.
- Improves chances of ROSC and survival.
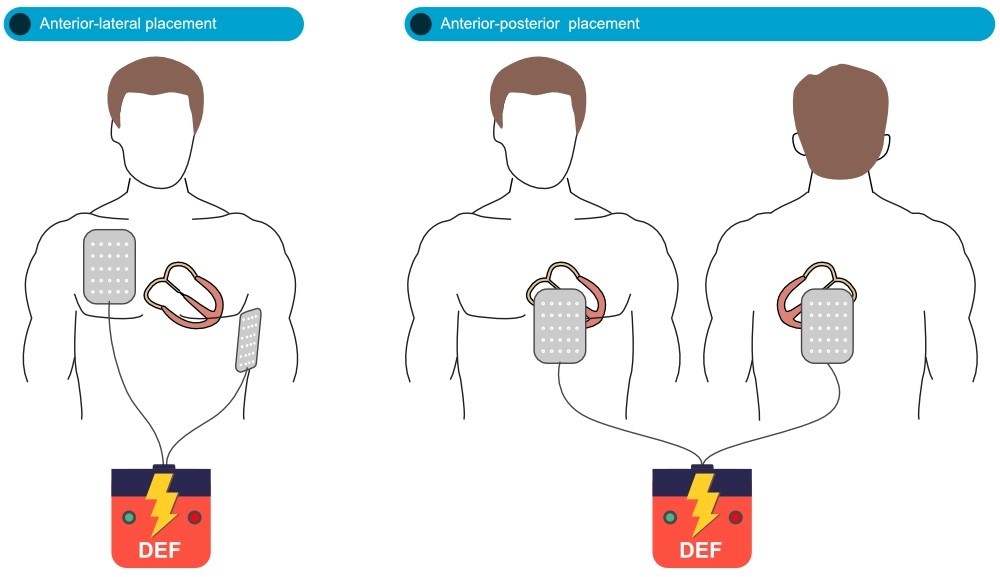
Anterolateral (AL) Pad Placement
"Antero" = front | "Lateral" = side
Pads "sandwich" the heart to direct current through the myocardium.
Anterior (right) pad: Just below the right clavicle, Right of the sternum, avoiding bony structures.
Lateral (left) pad: Over the left lower chest, Around V6 ECG lead level, near the mid-axillary line.
✅ Think: Right upper chest & left side of the chest, near the nipple line or slightly lower.
Anterior-Posterior (AP) Pad Placement & Vector Change Defibrillation (VCD)
What is VCD?
Vector Change Defibrillation (VCD) involves repositioning defibrillation pads from the anterolateral (AL) to anterior-posterior (AP) position after failed shocks. This changes the direction of current flow, offering another opportunity to achieve ROSC.
✅ Think: New vector, new chance to convert refractory VF/pulseless VT.
Why Use AP Placement?
- Redirects current through the heart’s vertical axis for deeper myocardial capture.
- Improves ROSC rates, especially in refractory VF/VT (supported by research like the DOSE-VF trial).
- Overcomes limitations like poor AL pad contact or challenging body habitus.
Anterior-Posterior Pad Placement
Anterior pad: Center of the chest, over the sternum or left precordium.
- Posterior pad: Mid-back, between the scapulae, just left of the spine.
✅ Avoid bony landmarks — ensure good skin contact and full adhesion.
Quick Tip:
Prepare AP pads early during cases of known or suspected refractory VF/pulseless VT. Switching vectors may be the key step toward successful defibrillation and ROSC.
General Pad Placement Tips:
- Avoid bone: Pads work best when placed over muscle/soft tissue.
- Hair removal: Quickly shave the area if the chest is very hairy.
- Dry the skin: Wet skin (sweat, rain) can interfere with pad adhesion and shock delivery.
- Firm pressure: Make sure pads are fully adhered to the skin.
- Correct distance: Pads should not be too close together to ensure the electrical current effectively captures the heart.
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management