August Tip of the Month - Heat Stress
As paramedics, understanding the nuances between heat illness, heat exhaustion, and heat stroke is crucial for effective and timely intervention, especially during the summer months. Heat-related emergencies range from mild heat illness to severe heat stroke, and recognizing the signs and symptoms can be life-saving. This tip of the month provides evidence-based education on these conditions, highlighting clinical exam findings and treatment considerations aligned with the Ontario Basic Life Support Patient Care Standards (BLS PCS).
Heat Illness:
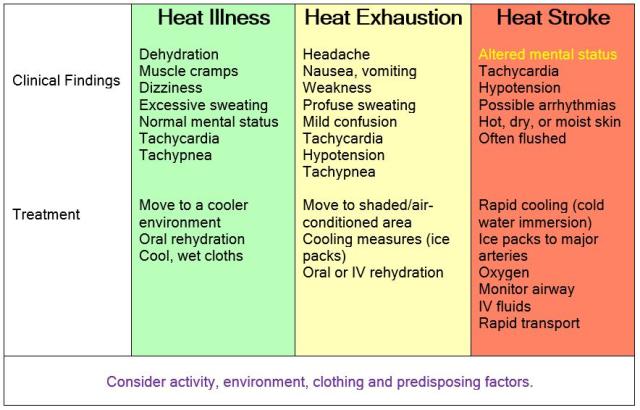
Heat illness encompasses a spectrum of conditions caused by elevated body temperature. Early signs include dehydration, muscle cramps, dizziness, and excessive sweating. Patients may present with increased heart rate and respiratory rate, but their mental status typically remains normal.
In cases of heat illness, patients may present with tachycardia, tachypnea, and moist, cool, pale skin. Treatment involves moving the patient to a cooler environment, providing oral rehydration if they are conscious and able to drink, and applying cool, wet cloths to the skin.
Heat Exhaustion:
Heat exhaustion is a more severe form of heat illness, characterized by significant fluid loss and electrolyte imbalance. Patients may exhibit symptoms such as headache, nausea, vomiting, weakness, and profuse sweating. Mental status changes, such as confusion or agitation, may occur but are usually mild.
In heat exhaustion, patients typically present with tachycardia, hypotension, tachypnea, and cool, clammy, pale skin. Treatment involves moving the patient to a shaded or air-conditioned area, initiating cooling measures by removing excess clothing and applying ice packs to the armpits, groin, and neck. Provide oral rehydration if possible, and consider intravenous fluids if oral intake is not tolerated or symptoms are severe.
Heat Stroke:
Heat stroke is a medical emergency characterized by a core body temperature above 40°C (104°F) and altered mental status, ranging from confusion to coma. This condition results from the failure of the body's thermoregulatory mechanisms and can lead to multi-organ failure if not promptly treated.
Heat stroke patients often exhibit tachycardia, hypotension, possible arrhythmias, and hot, dry, or moist flushed skin. The presence or absence of sweating does not determine severity. Altered mental status is the cardinal sign. Treatment priorities include rapid cooling by moving the patient to a cool environment, removing clothing, and using aggressive measures like cold water immersion or ice packs on major arteries. Administer oxygen, monitor the airway, establish IV access, and provide fluid resuscitation per Ontario BLS PCS guidelines. Rapid transport to the nearest emergency department is essential.
Key Points for Paramedics:
Early Recognition: Differentiate between heat illness, heat exhaustion, and heat stroke based on clinical presentation.
Aggressive Cooling: Initiate cooling measures promptly, with the goal of reducing the core temperature to prevent further damage. Think, “Cool first, Transport Second”.
Fluid Management: Rehydrate the patient appropriately, considering oral rehydration for mild cases and IV fluids for severe cases.
Monitor and Transport: Continuously monitor vital signs and mental status during transport. Be cognizant of if cooling procedures should be discontinued (e.g. Skin temp feels normal, generalized shivering develops, LOA normalized, etc.).
By adhering to these guidelines and incorporating evidence-based practices, paramedics can effectively manage heat-related emergencies, ensuring patient safety and optimal outcomes.
Stay cool and stay prepared!
References:
Ontario Ministry of Health. Basic Life Support Patient Care Standards (BLS PCS). (insert link to document for paramedic access)
National Association of EMS Physicians (NAEMSP) Clinical Guidelines.
More information:
Critical Levels – The Podcast (Episode 41|Heat Emergencies – Dr. Steve Sanders)
Previous Tips
-
Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management
-
April Tip of The Month - Paramedic resilience strategies; recognizing and managing burnout
-
March 2025 Tip of The Month - Identifying Intimate Partner Violence (IPV) in Prehospital Care