
Novemer Tip of The Month - STEMI 12 Lead Interpretation
Tip of the Month: Mastering 12-Lead ECG Interpretation of STEMI
Accurate interpretation of a 12-lead ECG is essential for paramedics in identifying ST-Elevation Myocardial Infarctions (STEMI) in the prehospital setting. While computerized interpretation tools offer valuable support, paramedics must be proficient in recognizing subtle signs, such as ST-segment elevation, reciprocal changes, and potential mimics like left bundle branch block or pericarditis. This skill enables paramedics to differentiate true STEMI from other conditions, ensuring timely and appropriate interventions, such as activating a STEMI bypass protocol or expediting transport to a PCI-capable facility, ultimately improving patient outcomes.
Areas of the Myocardium & Supply Vessels: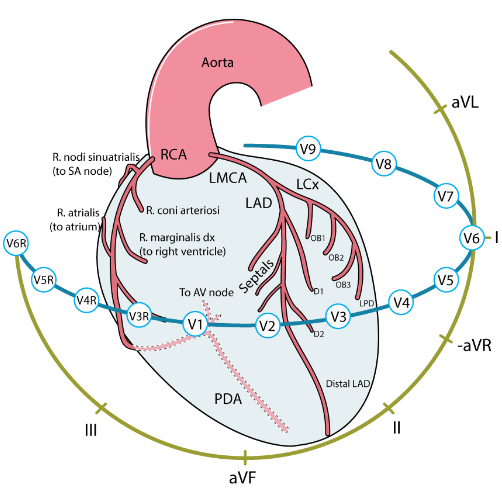
Reciprocal Changes: When ST elevation appears in leads that view one region of the heart, looking for ST depression in the opposite leads, known as reciprocal changes, is a critical step in confirming STEMI. Reciprocal changes strengthen the diagnosis by providing additional evidence that the observed ST elevation is due to an acute infarction rather than a benign mimic. For example, in an inferior STEMI (elevated ST segments in leads II, III, and aVF), reciprocal ST depression often appears in the high lateral leads (I and aVL). While not necessarily required, reciprocal changes may provide additional support.
- Confirm STEMI: Their presence supports that the ST elevation seen is a true myocardial infarction.
- Indicate infarct severity: More pronounced reciprocal changes can suggest a larger or more severe infarct, which can affect treatment urgency.
- Help distinguish from STEMI mimics: Conditions like pericarditis or early repolarization often show ST elevation but lack reciprocal depression, which aids in differentiating them from STEMI.
Potential Mimics:
Certain conditions can mimic STEMI on a 12-lead ECG, requiring careful analysis and clinical correlation to avoid misdiagnosis. Key mimics include:
Left Bundle Branch Block (LBBB): Characterized by a widened QRS complex (>120 ms), broad R waves in lateral leads (I, aVL, V5, V6), and discordant ST segments, which may show elevation that is not indicative of STEMI.
Ventricular Pacing: Produces a widened QRS complex, often with a left bundle branch block pattern and discordant ST-T changes, making it challenging to distinguish true ischemic changes.
Pericarditis: Shows diffuse ST elevation across multiple leads without reciprocal changes and often includes PR depression, particularly in lead II.
Early Repolarization: Presents with mild, concave ST elevation, usually in the precordial leads (V2–V5), with prominent J-point notching or slurring, typically without reciprocal changes.
Identifying these characteristics is essential for paramedics to differentiate between STEMI and its mimics, ensuring accurate diagnosis and appropriate intervention.
Available Treatment Options for Ischemia/Infarction:
Oxygen therapy (in accordance with BLS PCS)
Acetylsalicylic acid and nitroglycerin (where appropriate)
Rapid STEMI bypass activation to facilitate transport to a PCI-capable facility (in accordance with BLS PCS)
Risks of Relying on Computer Interpretations:
Computer-aided ECG interpretations offer valuable support but are not foolproof, sometimes resulting in false positives or negatives in STEMI detection. False positives (incorrect STEMI diagnosis) can occur with conditions like left bundle branch block (LBBB), early repolarization, or ventricular pacing, which mimic STEMI patterns and may mislead the algorithm. False negatives (missed STEMIs) may happen with subtle ischemic changes, such as isolated posterior or high lateral STEMIs, or when ST-elevation is just below the software's threshold limits.
Human oversight is crucial; paramedics must critically evaluate the computer-generated interpretations by incorporating ECG findings with the patient’s clinical presentation, symptom history, and physical exam. This approach enhances diagnostic accuracy and ensures that patients receive timely and appropriate care.
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management