
September Tip of the Month - Sepsis
Suspect Sepsis? Speak Up.
Sepsis, also known as Septicemia or blood poisoning, is a life-threatening condition caused by a dysregulated host response to infection. It’s most commonly triggered when bacteria from an infection elsewhere in the body enter the bloodstream, a condition called bacteremia. However, localized infections like pneumonia, urinary tract infections (UTIs), or skin infections can also provoke this systemic overreaction. While sepsis can occur in any patient, the elderly, immunocompromised and infants will be most susceptible.
Objective
By the end of this tip, paramedics will be able to identify early signs of sepsis and understand the importance of timely interventions and notification.
Scenario
You arrive at a call for “flu-like illness” The patient is febrile, tachycardic and hypotensive. Could this be something more than just the flu?
Key Content
- Sepsis is time-sensitive. Mortality increases with every hour of delayed recognition and treatment.
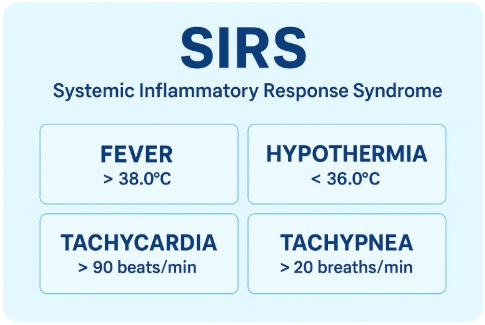
- Key indicators: Suspected or confirmed infection plus new or worsening vital sign abnormalities (i.e. fever, hypothermia, tachycardia, tachypnea, altered LOC, hypotension).
- Atypical Presentation: Not all patients with sepsis will appear critical ill. Maintain a high index of suspicion even if the patient doesn’t “look sick”.
- Tools such as SIRS can support recognition in the field.
Paramedic Role & Management Priorities: Early recognition and communication to receiving facilities can trigger hospital sepsis protocols and save lives.
- Oxygen therapy (if required)
- IV access & Fluid therapy (if authorized)
- BHP Patch Consideration: If sepsis is suspected and the patient is not hypotensive, consider patching to a BHP for direction regarding fluid administration.
- Pre-alert & Rapid Transport: Clearly communicate your suspicion of sepsis. Be aware of whether your receiving facility has a formal sepsis pre-alert process, but always ensure your suspicions are included in your handover.
Takeaway Message
If infection is known or suspected and vitals are abnormal, think sepsis and notify early.
Reflection
On your next call with fever or suspected infection, ask yourself: “Does this patient meet sepsis criteria?”
For More Information:
https://www.cmaj.ca/content/192/10/e230
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management