**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
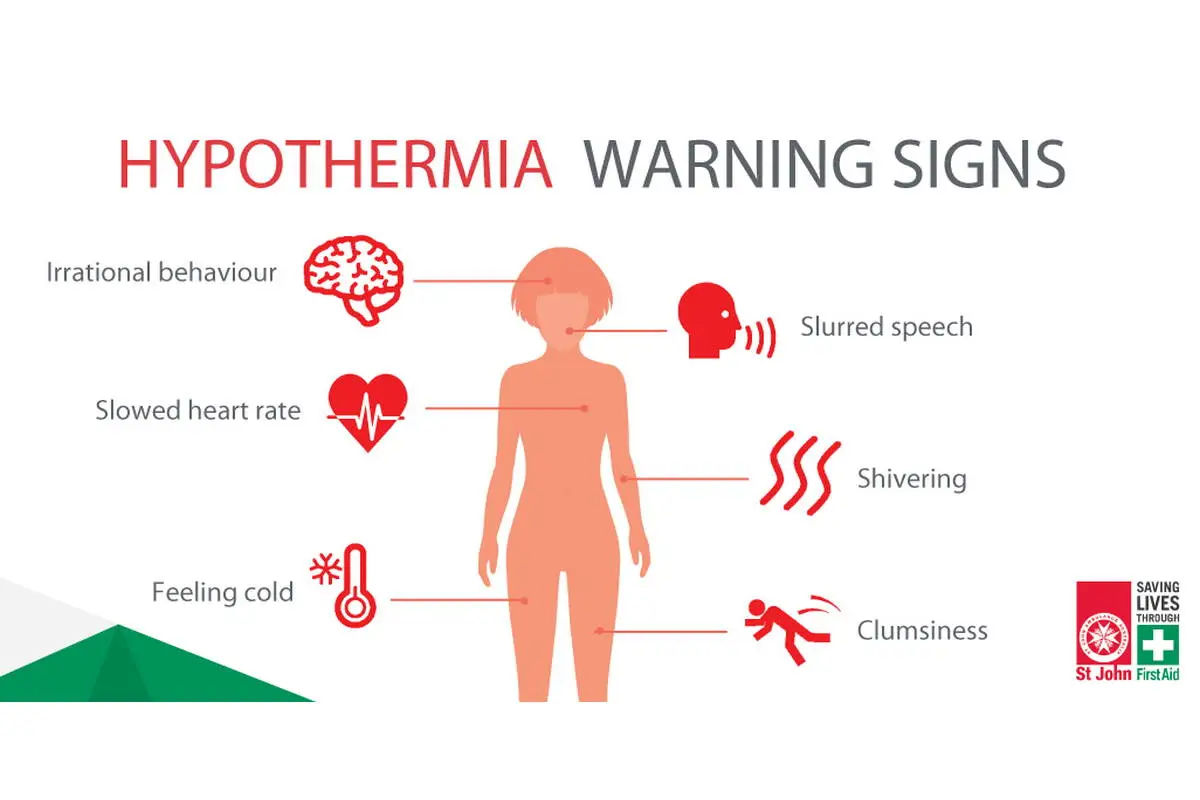
Hypothermia is a dangerous drop in core body temperature below 35°C, affecting the whole body, including the brain and organs, and can be fatal if untreated. Symptoms progress from shivering and confusion to loss of coordination, unconsciousness, and death, often caused by prolonged exposure to cold, wet, or windy conditions.
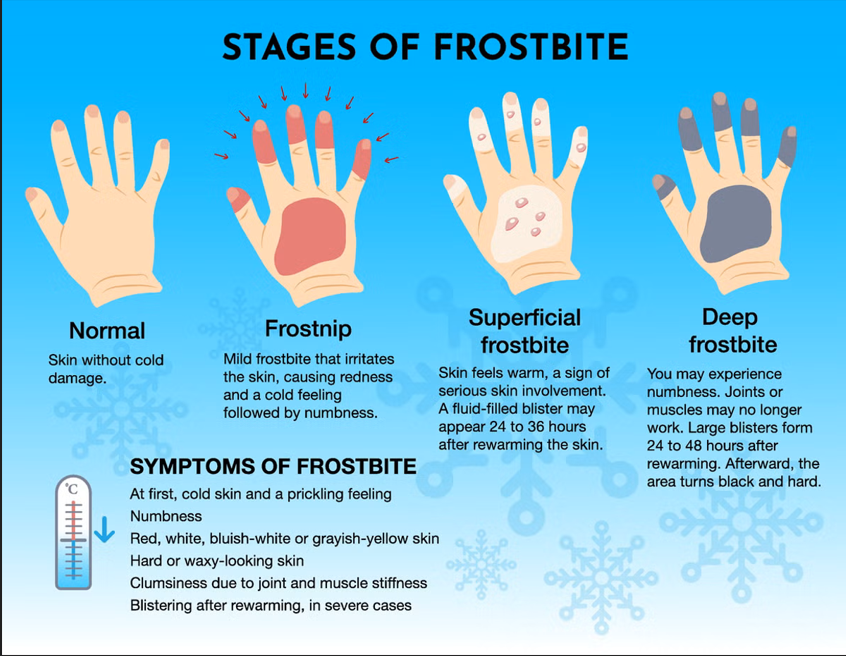
Frostbite is the freezing of skin and underlying tissues, usually in extremities like fingers, toes, nose, or ears. It causes localized numbness, pale or gray skin, and a hard or waxy feel, with severe cases leading to blisters or tissue death. While frostbite can cause permanent damage or amputation, it does not kill by itself.
Objective
Describe and differentiate the stages and clinical presentations of hypothermia and frostbite
Scenario
You attend the scene for a group of individuals with two of them requiring care, both feel cold to the touch.
One is a 46 year old male pt who is complaining of foot pain, upon a physical exam you note his toes are white and he has limited mobility. He is not dressed for the weather. The other is a 52 year old female who is lethargic with decreased mobility and states she has no complaints.
Which one of them do you suspect may be suffering from hypothermia?
Key Content
Stages of Hypothermia
|
Stage |
Patient Features |
Recommended Paramedic Actions |
|
Mild 32-35 ‘C |
Shivering, alert |
Passive rewarming, remove wet clothing, keep dry and insulated |
|
Moderate 28-32’C |
No shivering, altered mental status |
Active external rewarming (heat packs) warmed IV fluids, cardiac monitoring |
|
Severe < 28’C |
Unconscious, bradycardia, arrhythmia risk |
Gentle handling, cardiac monitoring, active external rewarming, remove wet clothes |
**Amendment** Cardiac Arrest Management
Early Transport - Focus on Reversible Causes
Rapid transport is a priority when:
- the arrest is presumed secondary to environmental exposure
- there is no obvious unsurvivalbe injury
- prioritize rapid transport to a facility capable of active core rewarming
CPR & Defibrillation (2025 AHA)
CPR:
- Provide high-quality CPR as per standard cardiac arrest care
- Avoid excessive interruptions during egress/extrication
- Handle the patient gently
Defibrillation
- It may be reasonable to deliver one defibrillation attempt if VF/pVT is present
- If unsucessful, further defibrillation should be deferred until core temp > 30 C
Epinephrine & Amiodarone Use (ACP)
- Withhold/defer the use of epinephrine and antiarrhythmics
- Drug metabolism is markedly reduced and may cause accumulation
- OMC may be contacted for consultation purposes.
Takeaway Message
Hypothermic patients can be challenging to assess because their signs and symptoms—such as altered mental status, bradycardia, hypotension, and shallow respirations—closely mimic those of other medical emergencies like overdose, stroke, or sepsis. This overlap can delay recognition and appropriate treatment, especially in urban environments where hypothermia may not be top of mind. Maintaining a high index of suspicion, especially in vulnerable or exposed populations, is key to early identification and care.
For further information regarding hypothermia and treatment please follow this link to watch a video with our very own Dr. Jon Smith.
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management