January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
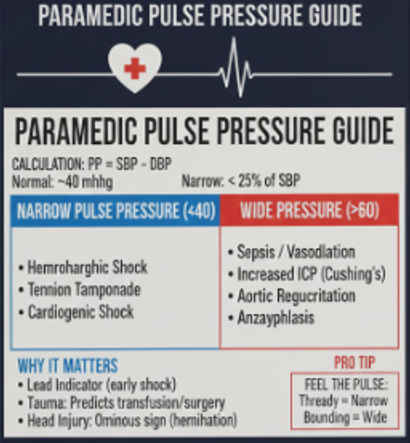
When assessing a patient in shock or with altered mental status, do not just look at the Systolic Blood Pressure (SBP). The Mean Arterial Pressure (MAP) is often a more accurate reflection of organ perfusion, particularly for the brain, kidneys, and heart. Pulse pressure (PP) is a vital sign that often tells a more compelling story about your patient’s hemodynamic status than the systolic blood pressure alone. In the prehospital environment, it serves as a "window" into stroke volume and systemic vascular resistance.
Objective
By the end of this tip, paramedics will be able to understand why MAP & PP matter and how to use it in the clinical setting.
Why MAP & PP Matter
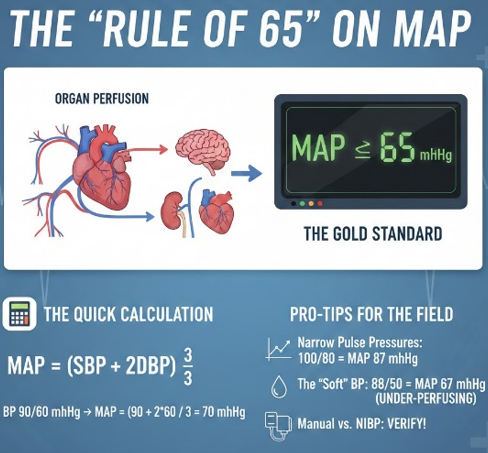
While SBP measures the "thump" of the heart, MAP represents the average pressure pushing blood through the systemic distal capillary beds during an entire cardiac cycle. Because the heart spends about two-thirds of its time in diastole (resting/filling), the MAP is weighted more heavily toward the diastolic pressure.
The Gold Standard: In most clinical settings, a MAP > 65 mmHg is the target to ensure adequate tissue perfusion & PP is 40mmHg.
The Quick Calculation
If your monitor does not display it, or you want to double-check the math, use this formula:
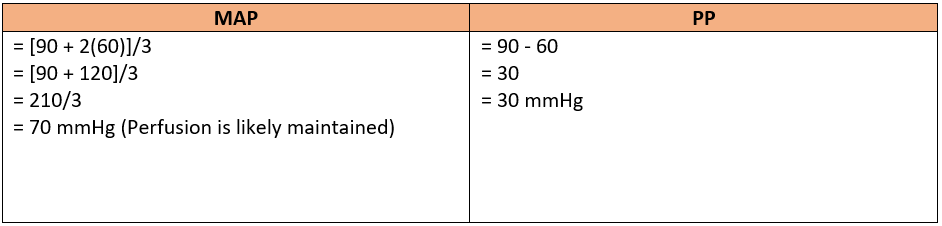
MAP = [SBP +2(DBP)]/3 PP = Systolic BP – Diastolic BP
Example: Your patient has a registered blood pressure of 90/60 mmHg.
Key Content
- Narrow Pulse Pressures: In early compensatory shock, a patient might have a "normal" systolic (e.g., 100/80), but their narrow pulse pressure results in a MAP that is borderline. Watch the trend, not just the single reading.
- Wide Pulse Pressures: In trauma, increased intracranial pressure (ICP) is part of Cushing’s Triad (widening PP, bradycardia & irregular respirations). In Sepsis, “warm shock” there is a massive vasodilation causing low diastolic BP.
- The "Soft" BP: If your patient is 88/50, their MAP is only 62 mmHg. Even though 88 systolic "feels" close to 90, they are likely under-perfusing critical organs.
- Manual vs. NIBP: If the automated cuff gives you a reading that does not match the patient's clinical picture (e.g., they are pale and diaphoretic but the MAP is 80), always take a manual BP to verify
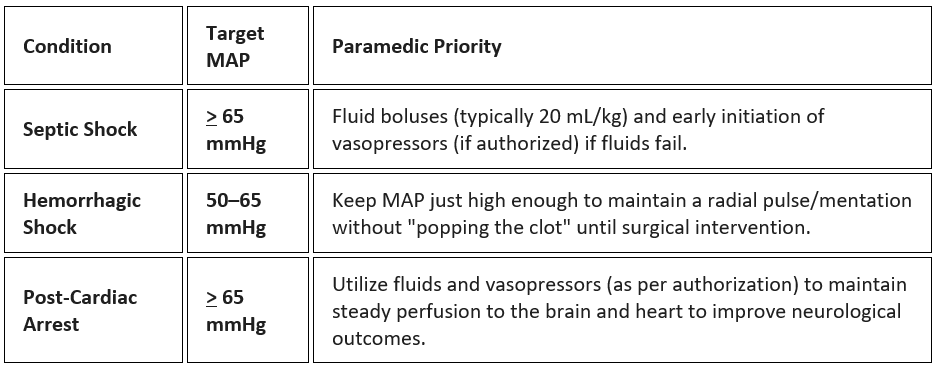
Paramedic Role & Management Priorities: Management priorities for MAP vary significantly depending on the underlying pathology.
Pulse pressure is often a lead indicator, whereas systolic blood pressure is a lag indicator.
- Catching "Compensated" Shock: A patient may have a "normal" BP of 110/90. Their systolic looks fine, but the pulse pressure is only 20 mmHg. This patient is likely in compensated shock and is about to crash.
- Trauma Decisions: Studies show that a narrow pulse pressure in trauma is an independent predictor of the need for massive transfusion and emergent surgery—even if the patient isn't hypotensive yet.
- Head Injury Alerts: If you see a rising systolic and a falling diastolic (widening PP) in a head-injured patient, it is a late and ominous sign of brain herniation.
Pro Tip: Don't just look at the monitor - feel the pulse. A "thready" pulse often correlates with narrow pulse pressure, while a "bounding" pulse correlates with a wide pulse pressure.
Takeaway Message
MAP is not just a number to document. Think about an underlying pathology and the use of MAP & PP to assist in informed decision making and the use of specific medial directives (eg. Cardiogenic shock medical directive) within your clinical ALS PCS directives.
Reflection
On your next cardiac or trauma call ask your self “Does my patient have adequate profusion with their BP?”
For More Information:
https://www.ncbi.nlm.nih.gov/books/NBK538226/
https://www.healthline.com/health/mean-arterial-pressure#how-to-calculate
Previous Tips
-
February Tip of the Month - Owning the Outcome: Ethics, Failure, and Legal Responsibility
-
January Tip of the Month - Mean Arterial Pressure "MAP" - The Rule of 65
-
**AMENDED** Winter Emergencies: Recognition and Care for Hypothermia and Frostbite
-
November Tip of the Month - Not "Just" the Flu: Recognizing High-Risk Respiratory Illness
-
October Tip of the Month - Diabetic Emergencies
-
September Tip of the Month - Sepsis
-
August Tip of the Month - Mass Casualty Incidents
-
July Tip of the Month - Breaking down Burns
-
June tip of the month - High-Quality CPR & Defibrillation
-
May Tip of the Month - Prehospital Trauma Management